During the late 18th and first half of the 19th centuries, the name Galt was widely recognized — and periodically the subject of gossip and controversy — among Virginians.
For three generations, from 1773 to 1862, the professional and private lives of members of the Galt family were inextricably entwined with Williamsburg’s Public Hospital for Persons of Insane and Disordered Minds, the first inpatient facility in America exclusively devoted to the treatment of people with mental illnesses.
For nearly 100 years, family members shaped the hospital’s everyday operations, policies and character. Well-educated and well-connected, the Galts contributed to the well-being of Williamsburg and played a significant role in laying the initial groundwork for a field of health care that continues to challenge and impact society.
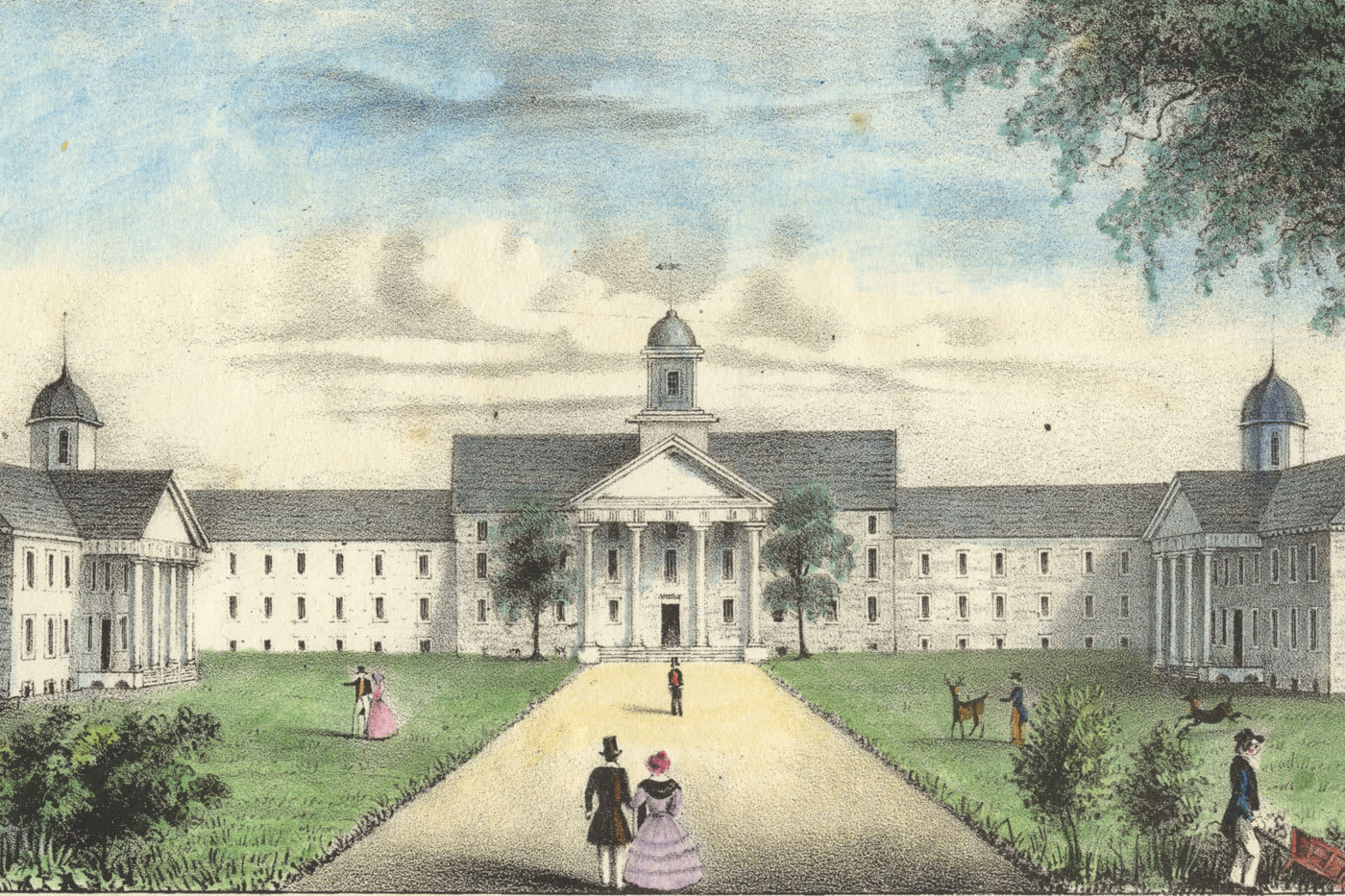
Located in the underdeveloped, sparsely populated western part of the community, but not far from William & Mary, the Public Hospital opened its doors in 1773 during a time of heightened hopes, fears, agitation and disquiet in the American colonies. Francis Fauquier, Virginia’s royal governor and a quintessential Enlightenment man, initially proposed such a facility to the House of Burgesses in 1766, shortly after the Stamp Act crisis, with its widespread protests, boycotts and riots, had been resolved.
The burgesses endorsed Fauquier’s proposition, and construction was completed seven years later. With Virginia and the other colonies sporadically in the throes of pre-Revolutionary upheaval, the creation of the Public Hospital in Williamsburg was a manifestation of widespread hope — and dread. Across the political spectrum, many feared that mental illness threatened the safety and stability of society. Yet many of the same people believed that the combination of science, rationality and good intentions could help cure these unsettling conditions.
When the hospital opened, the facility consisted of 24 “cells,” a meeting room for the board of directors, a large apartment for the keeper and matron, a laundry room, a substantial kitchen and a storage area. Because the hospital’s attending physician was required to come to the institution only once a week to see patients and advise the board on admissions and discharges, dedicated space for him was not considered necessary.
In light of the institution’s subsequent history, the criteria for admissions are especially noteworthy: The hospital was to admit only persons who were judged either curable or dangerous. Harmless vagrants, destitute beggars and nonviolent persons who suffered from chronic or degenerative conditions were not considered proper subjects for admittance. The hospital was established to intervene only during a severe mental crisis to provide immediate, short-term services and then discharge the patient. It was not a facility for persons with long-term degenerative conditions.

Family Ties
Samuel Galt, a Scot-Irish immigrant, moved to Williamsburg in the mid-1740s. A goldsmith by trade, he also served as keeper of the public gaol from 1759 to 1761.
Samuel’s son James ushered in the family’s tie to the hospital. He followed his father as keeper of the gaol for five years, and in 1773, when the hospital opened, he was appointed its first keeper, and his wife, Mary, was the matron. Together they were responsible not only for day-to-day operations but also for patient care.
James Galt’s younger brother, Dr. John Minson Galt, joined the hospital’s workforce in 1795 when he was appointed its part-time attending physician. Born and raised in Williamsburg, John Minson attended William & Mary and then studied medicine in London, Edinburgh and Paris.
When John Minson Galt died in 1808, he was succeeded by his son, Dr. Alexander Dickie Galt, who, after graduating from William & Mary, also received medical training in London. For over three decades, until his death in 1841, Alexander Dickie Galt served as the hospital’s attending physician.
Approaches to Treatment
Given their era, the Galt doctors were impressively trained and community-minded — Alexander Dickie Galt also served on William & Mary’s board — but their treatment regimen was limited and lacking mostly because the outlook, understanding and therapeutic approaches at that time were at best in embryonic stage. On top of that, Williamsburg was increasingly becoming a backwater community in the decades after the Revolution.
Father and son were relatively conventional in attitude and action. Medically they relied on purgatives to evacuate the bowels, emetics to cause vomiting, anti-inflammatories to reduce swelling, occasionally opium to induce calm, periodic warm baths to soothe, sometimes modest blistering on the back of the neck for fevers, very rarely bleeding and not infrequently “considerable” amounts of whiskey or “small” quantities of rum.
Activities in the hospital were few. Patients mostly remained in their cells day and night, mealtimes included. For a time during the late 1820s and the first half of the 1830s, Dickie Galt tried to lessen the monotony of everyday life by offering some patients opportunities to do small outdoor tasks. Eventually he brought approximately a dozen men to his farm to work during the day.
Relatively soon, though, Dickie Galt came under intense pressure from his
relative Mary Arnet Godwin Galt, the institution’s longtime matron for women and a strong patient advocate, as well as to a legislative committee that came to Williamsburg from Richmond to investigate hospital conditions and practices. In 1836, Dickie Galt resigned his post.
Some 60 years after the institution opened with optimistic expectations, the situation inside the facility was bleak. Staff morale was low, initiative virtually nonexistent and patient idleness commonplace.
“The hospital exhibits too much the appearance of a well regulated prison, where the prisoners are well fed and clothed, and excluded from all rational employment or amusement,” the investigating committee from Richmond concluded. Of 59 patients confined to the facility in late 1834, nearly one-third had been there for more than 10 years. During that same year, only three patients were released. For the others, the outlook was grim. The hospital was inexorably becoming a glum place for the custodial care of patients with chronic mental illnesses.
A New Approach
Enter Dr. John Minson Galt II, grandson of one attending physician, son of another.
Born in Williamsburg in 1819 — some 75 years after his great-grandfather had moved there — young John Minson grew up in relative comfort, encircled by immediate and extended kin as well as a wide range of familiar townspeople.
Athletic, a voracious reader, gifted in languages and fascinated by botany, he graduated from William & Mary and traveled to Philadelphia to study at the prestigious Medical College of the University of Pennsylvania.
Notwithstanding bouts of loneliness and dyspepsia and a deep sense of social discomfort that he feared could be misinterpreted as rudeness and churlishness, young John Minson explored Philadelphia’s bustling, diverse and cosmopolitan culture, but his strong attachments to family, community and duty eventually prevailed. After some nagging hesitation and vaguely articulated reservations about his future path upon graduation, he came home to familiar people and accustomed ways.
In 1841, the young doctor was appointed the hospital’s superintendent, a new position in which he served simultaneously as a full-time physician and also its top administrator. Previously, hospital doctors had been part-time employees who maintained a private practice in town.
Although young Galt experienced some qualms about accepting this demanding position, he fully immersed himself in the work. Open to innovative ideas, he became an agent for change, revitalization and new hope at the dreary institution in the quiet town.
At the hospital, Galt created weaving and sewing rooms, a carpentry shop and a library to engage patients in diverse activities. He purchased an array of musical instruments and games and hired attendants whose primary responsibility was to befriend and engage patients in conversation. He sought to reduce — initially, to eliminate — the use of physical restraints. He did away with abrasive drugs and increased the use of soothing ones. Patients were encouraged to spend time outdoors, walking the well-kept grounds and puttering in the gardens. Evening lectures, recreational gatherings and concerts were organized. Galt also markedly upgraded the condition of the physical plant, increased the number of residential buildings to minimize crowding, improved the quality of patients’ clothing and acquired comfortable furniture for bedrooms and activity areas.
In contrast to his predecessors, Galt communicated with colleagues at similar institutions throughout the country, visited mental health hospitals in other states to further educate himself and assiduously read about such hospitals in Europe. In 1844, he was one of 13 founders of the Association of Medical Superintendents of American Institutions for the Insane, a forerunner of the American Psychiatric Association. He also contributed relatively frequently to the association’s professional publication, The American Journal of Insanity.
In one of the hospital’s annual reports, Galt acknowledged that notwithstanding his considerable efforts and experience, mental illness remained an “awful mystery”; in another, he conceded that on the hospital wards “practice invariably falls short of theory.”
To help with his mounting duties, he enlisted his sister Sarah Maria Galt to assist in an unpaid capacity with preparing public documents, extending small kindnesses to patients and corresponding with their families. In 1850, he hired his cousin, close friend and associate, Dr. John Galt Williamson, to join the hospital’s staff as a full-time assistant physician with hopes of alleviating the vast workload and improving services.
A Bold Proposal
Nevertheless, the population of long-term, chronic residents continued to climb; the number of discharged patients remained small; and Galt’s habitual use of laudanum, an opiate, to soothe himself, increased steadily during the 1850s. While his confidence in the overall effectiveness of the hospital regimen wavered, Galt’s commitment and devotion to patients did not.
Finally in 1857, Galt went public with his most audacious and revolutionary proposal. A few years earlier he had forthrightly stated that hospitalized patients are “our brethren” who are more like “ordinary persons” than not.
Now he took another step in that direction by publicly declaring, “A large number of the insane, instead of rusting out their lives in the confines of some vast asylum should be placed as boarders with persons in the neighboring community.”
Other patients, he proposed, could work in town during the day but return to the hospital for the night. Still others, who were convalescing or harmless, could live and labor at a nearby farm administered by the institution. Only patients who required constant care needed to stay full time in the facility.
The proposal received harsh responses from Galt’s colleagues at other mental health hospitals in the country, and townspeople were alarmed. While his family remained stalwart supporters, Galt became professionally isolated.
Five years later, in mid-1862, when Union troops captured Williamsburg and seized the facility, Galt, a Confederate supporter, was distraught and became ill. To calm his upset stomach and frayed nerves, he self-administered a large amount of laudanum, the opiate on which he had become increasingly dependent. He died at age 43 after 21 years serving hospital patients and his community.
Viewed from a modern-day perspective, the doctor was burned out. A few years before his death, he wrote, “Men walk in shadows and darkness whilst an inexorable abyss lies yawning at their feet.”
At minimum, Galt could not figure out how to navigate the subtle and intricate transitions of his dawning middle age. The personal and professional choices he had made in early adulthood eventually collided with the challenges he faced in his late 30s. Wracked by feelings of inadequacy and often professionally isolated, Galt seemed increasingly haunted — and broken-hearted.
None of Dr. Alexander Dickie Galt’s four children ever married or had progeny. When Sarah Maria died in 1880, that wing of the family came to an unheralded end. The hospital continued, eventually in another part of town. To this day it serves patients, but that part of the Galt family vanished, though it left behind a legacy for a facility whose stated mission today is to demonstrate and encourage compassion to empower patients in their recovery.